Brachycephalic Obstructive Airway Syndrome surgery (BOAS) Pug, 2y, female
Case 4 - Peggy
Peggy presented with a history of snoring and exercise-induced respiratory difficulty (see video below). No episodes of regurgitation were reported. Following a comprehensive evaluation, she was deemed a good candidate for surgical correction of the nares due to moderate stenotic conformation (Fig. 1), with probable elongation of the soft palate to be assessed and confirmed during induction.
Staphylectomy
During induction, the soft palate was observed to be markedly elongated, extending cranially beyond the epiglottic cartilage and causing near-complete obstruction of the laryngeal inlet, severely compromising airflow.
A surgical cut line was pre-marked using a sterile marker during the initial assessment (Fig. 3).
Lateral sutures were pre-placed prior to resection, and a cut–suture–cut–suture technique was employed to ensure precise apposition of the nasopharyngeal and oropharyngeal mucosa.
Closure was achieved using a simple continuous pattern with 2-metric Monocryl.
Tonsils: Normal in size and coloration, remaining within the crypts
Laryngeal saccules: Normal; no eversion or prolapse observed
Following the staphylectomy, the laryngeal inlet was visibly clear, with the endotracheal tube no longer surrounded by the soft palate (Fig. 4)
Nasoplasty
A local block was performed at the nares using a combination of adrenaline and 2% lidocaine (1/9). This provided immediate postoperative analgesia and excellent hemostasis.
A vertical wedge resection of the dorsal alar folds was carried out with a No. 11 scalpel blade following infiltration of 0.3 mL of the adrenaline/lidocaine mixture into each fold (Fig. 2).
Bleeding was minimal and controlled easily. Closure was completed using simple interrupted sutures, with two stitches placed in the internal ventral nasal mucosa for optimal aposition and symmetry.
No active bleeding was observed at the soft palate surgical site prior to recovery.
Hospitalisation & Recovery
Recovery was largely uneventful. Mild upper respiratory noises were noted, attributed to mucus and mild pharyngeal secretions.
Peggy remained calm, comfortable, and was breathing with a closed mouth.
Postoperative Plan
Overnight hospitalization with strict monitoring : Peggy recovered smoothly from surgery and was deemed stable at the time of discharge. She was transferred to a nearby veterinary facility offering overnight (OOH) monitoring to ensure continued supervision during the immediate postoperative period.
Close observation of airway patency and respiratory effort
Continued supportive care to manage potential postoperative swelling or obstruction
*This case demonstrates that procedures such as staphylectomy and nasoplasty can be successfully performed in general practice settings. With proper planning and collaboration with OOH services for postoperative care, patients can receive comprehensive treatment without compromising safety or outcomes.




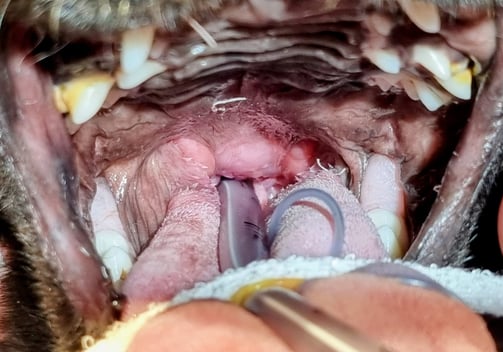
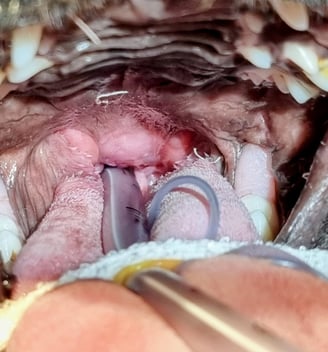
Fig. 1
Fig. 2
Fig. 3
Fig. 4


Sound ON!
Peggy before
Peggy after
Troya Surgery
Specialized mobile surgical services for veterinary practices.
Contact details
Email: troya.surgery@gmail.com
Telephone: 0771 625 1040
© 2024. All rights reserved.
WhatsApp: +44 771625 1040